Alzheimer’s in Military Veterans
By:
Dr. Carol Henricks
On
24/07/2025Summary:
Is Alzheimer’s dementia an unavoidable consequence of aging, or is it a treatable condition ? Statistically a higher
percentage of military veterans, first responders and professional athletes will be diagnosed with “Alzheimer’s Disease”
and at a younger age than the rest of the population. What is driving this trend ?

Many neurological conditions were first named and categorized at a time when sophisticated testing was unavailable. The term Alzheimer’s disease was first used by Alois Alzheimer in 1906 when the term was used to describe a person in their early 50’s who suffered memory and cognitive loss that rapidly progressed. Patient evaluation at that time was based solely on a complete neurological exam that was repeated at intervals. A group of physicians would gather, and the patient would be questioned and examined. Notes would be taken. Months later this would be repeated. There was no “medical testing” as we do today. There was no brain imaging. It was purely a
clinical diagnosis, a clinical description.

Traditionally there has been a general assumption of cognitive decline withageing but exceptions were noted. There were people who remained sharp and competent into their 90’s and beyond. This observation opened the door for pharmaceutical interventions. Cognex or
Tacrine Hydrochloride was the first medication used to treat short term memory(STM)deficits by increasing levels of the neurotransmitter acetylcholine in the temporal lobe (memory processing center) of the brain. Cognex was first available in 1993. Cognex was developed to treat Alzheimer’s Disease, and a diagnosis of AD was necessary to receive the prescription. Some memorybenefits were noted, and every person with memory problems wanted the opportunity to try the drug. So the label of Alzheimer’s Disease became pervasive.
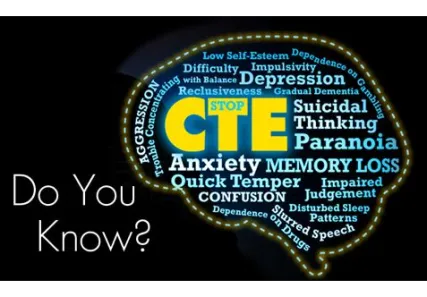
Dementia is cognitive loss in 2 or more areas of function. But what
conditions present as (Alzheimer’s) dementia? Recall that
Mike Webster, the football player featured in the movie
“Concussion”, presented with clinical symptoms of Alzheimer's Dementia. Neuropathologicallyat autopsy Mike Webster
was diagnosed with chronic traumatic encephalopathy
(CTE) after a lifetime of concussions throughout his professional career.
Mike Webster had plaques and neurofibrillary tangles throughout his brain. Many kinds of injuries may initiate progressive neuropathology and result in progressive brain cell dysfunction and brain cell death including blunt
trauma (concussion / Directed Energy Weapon / blast injury), inflammation, toxicity / drugs / alcohol, nutritional
deficiency, neurohormonal dysregulation, genetic dysfunction, infection, ischemia, anoxia hypoxia (sleep apnea),
sleep disturbance, and intracerebral bleed. This is not an exhaustive list. All of these brain injuries, when they are not resolved, result in cellular injury and progressive brain cell dysfunction or death: a neurodegenerative process that leads to progressive cognitive and functional disability. All these forms of insult and injury are, to a certain extent, treatable conditions.

When brain cells die, they leave behind plaques and tangles. Neurofibrillary tangles develop when tau proteins dissociate from the microtubular infrastructure of
the cell, and clump together. Plaques develop from
abnormal buildup of proteins in the brain. Plaques and tangles, which have been described as being present in Alzheimer’s patients, are present in the brains of many people at brain autopsy. Plaques and tangles are present in patients that do not have dementia. Our immune
system clears plaques and tangles from the brain through astrocytes, microglia, CSF clearing, enzyme
degradation, and other processes. Are plaques and tangles the final common product or residual from brain
cell injury and death and patients that have more plaques and tangles have suffered more injury and more cell death ?
Could the amount of debris that needs to be cleared
overwhelm the system leaving more plaques and tangles behind in patients that have been more injured ?
Certainly plaques and tangles are not a unique
neuropathology associated with a specific disease condition. Our brain health at any point in time is a
product of illness and injury that we have experienced
during our life. A focus on monitoring and treating
these injurious pathologies will lead to the best long
term cognitive outcome.
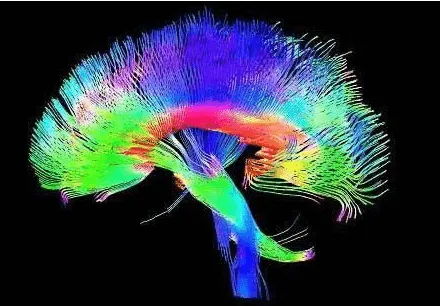
How can the brain be healed ? Hyperbaric oxygen thereapy (HBOT)
improves cellular health, causes neurogenesis (cellular differentiation) heals fiber tracts, promotes detoxification, helps to fight infection and is anti
inflammatory. Detoxification protocols can be used.Hormone replacement therapy is critical. Nutritional optimization is healing. Sleep apnea can be treated. Brain health is mental health. Preventive medicine practices
should be used to preserve our brain health throughout life !
